Ulcerative colitis: Treatment and pain relief
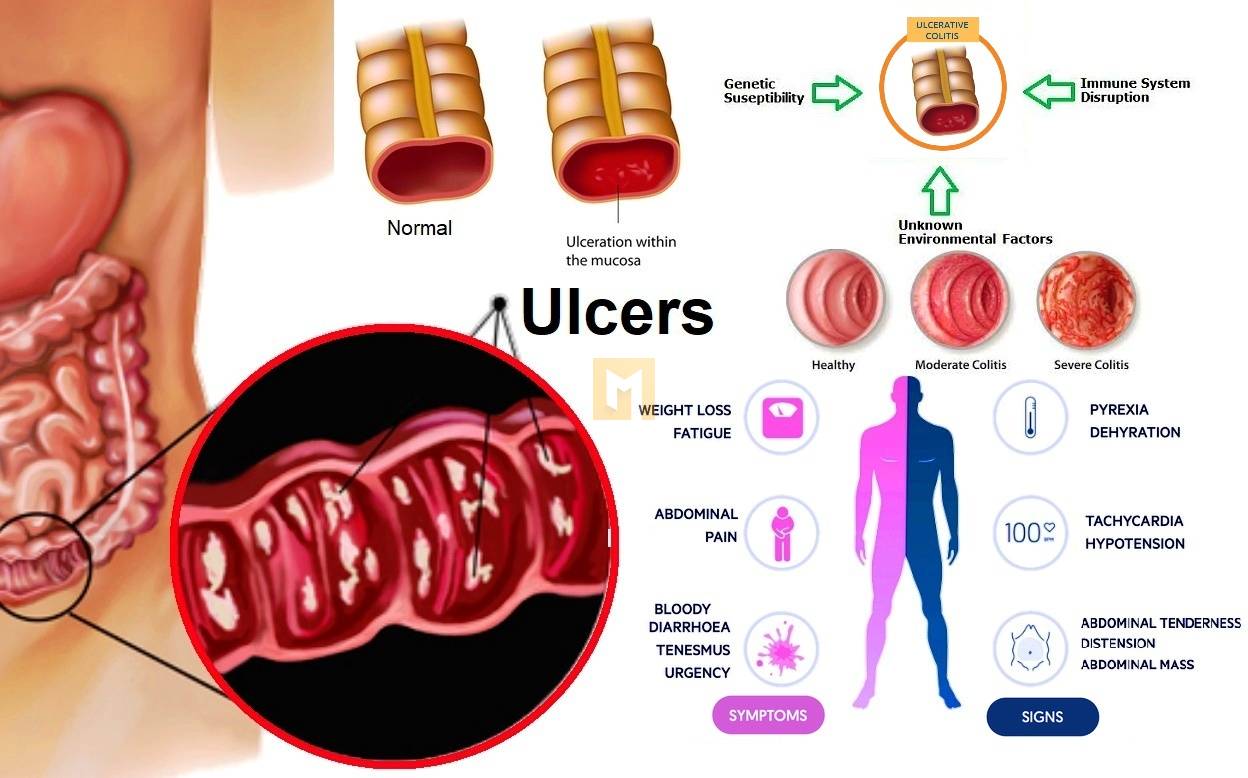
Ulcerative colitis (UC) is a chronic inflammatory disease of the lower gastrointestinal tract (GIT). This is because the symptoms get worse and the person experiences diarrhea, bloating, discomfort and pain. These periods are called bursts.
UC is a type of inflammatory bowel disease (IBD) which also includes Crohn’s disease and microscopic colitis. About 600,000 to 900,000 people in the United States have UC.
Like other IBD disorders, UC fluctuates between periods of remission with few or no symptoms and periods of exacerbation, which healthcare professionals refer to as exacerbations. Symptoms include diarrhea, blood or pus in the stool, and abdominal pain.
According to the Crohn’s and Colitis Foundation (CCF), 33% of people with UC have chronic abdominal pain. For this reason, UC pain management is often an important part of a person’s treatment plan.
This article describes strategies for treating and managing UC that can help reduce relapse and reduce pain.
Treatment and management
Pain relief from UC can be achieved through lifestyle changes and medical interventions that help relieve inflammatory pain.
Medications may include medications that help reduce inflammation in ulcerative colitis and medications that relieve pain.
Depending on the individual’s level of pain and discomfort, a combination of some of these options may be necessary. A person should talk to their doctor about the pain management and treatment options that are best for them.
People can try the following strategies to reduce swelling and pain:
Change your eating habits
People with ulcerative colitis may want to avoid certain foods because some foods can cause pain and discomfort.
Possible trigger foods include:
Indigestible fiber, such as raw or cruciferous vegetables, nuts, whole grains, and fruits with seeds and skins
Dairy products
Sweets and foods that contain sugars that are difficult to digest, such as sorbitol or mannitol
- Fat food
- alcohol
- caffeine
- hot food
To reduce pain crises, the CCF suggests that people:
- Eat small amounts 4-6 times a day.
- Stay hydrated
- Drink slowly
Planning meals ahead of time and using simple cooking methods like baking, steaming, braising, or boiling can help you choose less spicy foods.
However, studies have not conclusively shown that some foods cause ulcerative colitis symptoms. Further studies are currently underway. When people choose to avoid certain food groups, they may not be getting enough nutrition.
For this reason, the National Institute of Diabetes and Digestive and Kidney Diseases recommends that people eat a balanced diet.
You should also consult your doctor to determine which dosage is best for you. Your doctor will help you decide if you really need to remove certain foods from your diet.
Improved mental health
Stress, anxiety and depression can also contribute to the painful symptoms of IBD.
Studies have shown that people with mood disorders and Crohn’s disease may be more susceptible to flare-ups than those with ulcerative colitis.
However, 15 studies of more than 5,000 people with IBD, including UC, have found an association between mood disturbances and abdominal pain.
Therefore, learning and using stress management skills can help reduce the likelihood of a painful relapse.
Take probiotics
Probiotics are live bacteria that benefit the human body. They may benefit digestion by balancing the human gut microbiome, the natural bacterial population of the human digestive tract.
You can get probiotics as a supplement or by eating probiotic foods.
Probiotics may reduce the pain of inflammation in UC. However, the number of studies examining whether probiotics can help relieve ulcerative colitis symptoms is small and the results are inconclusive.
There is some evidence of improvement in symptoms in mild to moderate ulcerative colitis following fecal microbiota transplantation. While more research is needed, existing research supports the idea that IBD symptoms may be related to gut bacteria.
To take the pill
Medication may be necessary if preventative strategies are insufficient.
Some medications help reduce pain while treating the inflammatory process of the disease. Other medications can reduce the pain, but they do not treat the underlying cause of the pain.
Drugs that target ulcerative colitis
First-line treatment for UC is usually a 5-aminosalicylic acid (5-ASA) drug such as sulfasalazine or mesalamine. This medication contains 5-ASA, which reduces intestinal inflammation.
A person can take this medicine orally or rectally. Studies have shown that this drug reduces the symptoms of ulcerative colitis by about 50%.
Other medications that directly treat the inflammatory process in UC include:
- Corticosteroid
- immunomodulator
- Organic products
- Painkillers
You can also take pain relievers to ease the discomfort you feel during the burn.
These drugs:
Opioids: Opioids such as oxycodone and Vicodin relieve the symptoms of ulcerative colitis. However, opioids should be used with caution as they can lead to physical dependence and addiction.
Antidepressants: Some antidepressants improve intestinal symptoms by affecting serotonin in the human body.
Non-steroidal anti-inflammatory drugs (NSAIDs): NSAIDs such as ibuprofen and naproxen relieve pain, but can also damage the gastrointestinal tract. For this reason, it may not be the most appropriate option for IBD patients.
Medicinal Cannabis: Helps relieve pain. However, research on medical cannabis is still limited and the legal status of medical cannabis varies from state to state.
Medicines that relieve bolus cramps may also help.
Causes of UC Pain
The exact cause of ulcerative colitis varies from person to person and inflammation to inflammation. Finding the exact cause of pain is one of the most important steps in treating pain.
People with ulcerative colitis may experience the following types of pain:
- Abdominal pain due to diarrhea or appendicitis
- Scar tissue pain in the abdominal cavity due to repeated inflammation
- Pain from digestion of food through inflamed tissues
- Visual hypersensitivity with hypersensitivity of the enteric nerves
- Pain on the left side of the stomach due to left-sided colitis
In some cases, people with UC may also experience joint pain and painful itching in the abdomen.
Diagnose
To diagnose ulcerative colitis, doctors start with a thorough physical exam. They ask about symptoms, general health and lifestyle, diet, family medical history, and other factors that help make a diagnosis.
The next step is usually a blood test and a stool sample for testing. These tests help rule out other causes of a person’s symptoms, such as a viral or bacterial infection. A blood test can also help determine if there is bleeding in the intestines.
In addition, x-rays of the gastrointestinal tract may be required.
Your doctor may order an endoscopy or colonoscopy.