Health
Autoimmune arthritis: Types, symptoms, and treatment
Autoimmune arthritis: Types, symptoms, and treatment
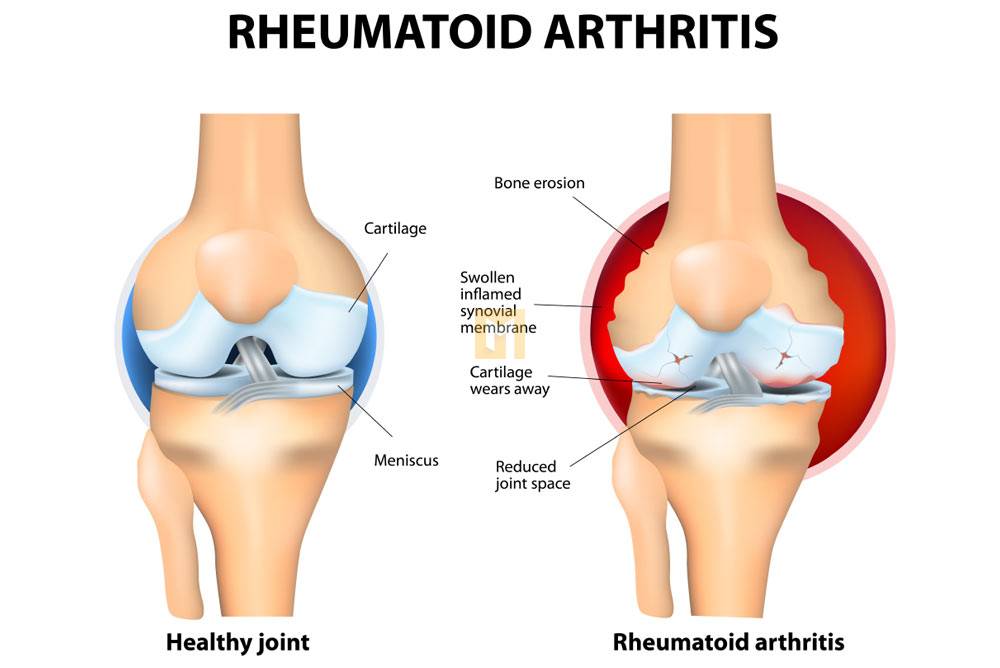
Autoimmune arthritis refers to a type of arthritis in which a person’s immune system attacks its own body.
When the body’s immune system attacks, arthritis is the result.
There are over 100 types of arthritis, each with different symptoms. Rheumatoid arthritis and psoriatic arthritis are the most common forms of autoimmune arthritis.
This article takes a closer look at autoimmune arthritis, identifies common symptoms, and outlines some of the treatments currently available to combat the arthritis associated with osteoarthritis.
Types of autoimmune arthritis
This list is by no means exhaustive, but it represents some of the most common forms of autoimmune arthritis.
RA: The most common form of autoimmune arthritis, RA usually causes swelling and pain in the hands, feet, and wrists. An estimated 1.3 million people in the United States suffer from rheumatoid arthritis, of which 75% are women.
Spondyloarthritis: This is a term that refers to a group of arthritis-related conditions that affect the spine and joints. Some common types include ankylosing spondylitis, axial spondyloarthritis, reactive arthritis, PsA, and enteroarthritis.
Juvenile arthritis: Juvenile arthritis affects an estimated 300,000 children in the United States and can cause joint pain, burning eyes, fever, and rash. Other names include juvenile idiopathic arthritis, juvenile chronic arthritis, and juvenile rheumatoid arthritis.
Rheumatoid arthritis: Rheumatoid arthritis is a rare form of arthritis that causes inflammation around the joints. Alternating arthritis often affects the areas around the fingers, wrists and knees, causing symptoms such as pain, swelling, stiffness and fever.
Each of these conditions can cause significant joint discomfort and swelling.
Symptoms of autoimmune arthritis
Common symptoms associated with autoimmune arthritis include:
- Heat
- joint pain
- string of arrows
- swelling
- weakness
Specific symptoms depend on the type of autoimmune arthritis.
For example, PsA can cause a condition called enthesitis, which causes painful points in areas where ligaments and tendons attach to the bone. These symptoms often occur behind the heel and around the elbow.
Risk factors
Experts believe that genes can affect a person’s chances of developing autoimmune arthritis. However, other risk factors for autoimmune arthritis vary depending on the type of arthritis.
For example, some studies suggest that periodontal disease, also known as periodontal disease, may be associated with an increased risk of developing rheumatoid arthritis.
Environmental factors can also be a factor. Factors that may contribute to autoimmune arthritis include:
- early exposure to toxins, such as those in cigarette smoke
- smoking cigarettes
- obesity
Gender can affect your risk level for certain types of arthritis. For example, women are two to three times more likely to develop RA than men.
Examples of diagnostic tests for autoimmune arthritis include reliable sources.
Imaging scans such as X-rays, CT scans, MRI scans, and musculoskeletal ultrasounds can identify areas of joint damage.
Blood tests, including red blood cell count, rheumatoid factor, specific peptide antibodies, and markers of inflammation such as erythrocyte sedimentation rate and C-reactive protein (CRP) levels.
Printed models that doctors can use to diagnose underlying conditions such as psoriasis.
However, no single test can provide a definitive diagnosis of the type of autoimmune arthritis. Diagnosis often involves a series of tests to rule out other conditions and other types of arthritis.
Process
When recommending an autoimmune arthritis treatment plan, doctors consider a person’s symptoms, type of arthritis, and overall health.
Treatment
Some people with mild autoimmune arthritis may benefit from taking nonsteroidal anti-inflammatory drugs. These include ibuprofen (Advil) and naproxen (Aleve).
For other types of arthritis, doctors may prescribe medications known as disease-modifying anti-rheumatic drugs (DMARDs).
Examples of DMARDs are:
- Sulfasalazine (Azulfidine)
- Methotrexate (Leometrix)
- Leflunomide (Arva)
- Hydroxychloroquine (Plaquenil)
- Janus kinase (JAK) inhibitors such as baricitinib (Olumiant), tofacitinib (Xeljanz), updacitinib (Rinvoq).
If DMARDs are not effective in treating autoimmune arthritis, your doctor may prescribe biologic response modifiers, or “biologic agents.” These drugs can cause symptoms of autoimmune arthritis. It inhibits the circulation of an active immune system.
Examples of biological agents include reliable sources.
- Abatacept (Orencia)
- Tocilizumab (Actemra)
- Rituximab (Rituxan)
- Tumor necrosis factor alpha inhibitors such as etanercept (Enbrel), infliximab (Remicade), adalimumab (Humira), certolizumab pegol (Cimzia), and golimumab (Samponi).
- Interleukin-17 inhibitors, including secukinumab (Cosentyx).
- Interleukin-23 inhibitors such as ustekinumab (Stelara), guselkumab (Trenfia), tildrakizumab (Ilmya), linsankizumab (Skyligy).
In some cases, these drugs can be taken with DMARDs, especially methotrexate.
Medicines have side effects, which can cause problems of their own. For example, there are DMARDs and biologic immunosuppressants that make people more susceptible to infections.
Lifestyle changes
In addition to treating autoimmune arthritis, your doctor may recommend lifestyle changes and options that can help people with autoimmune disorders.
Examples of lifestyle strategies for managing autoimmune arthritis include authoritative sources.
Regular exercise: Certain types of physical activity can improve joint range of motion. Walking, water aerobics, and other low-impact aerobic exercise are especially helpful.
Quit smoking if applicable: Smoking can worsen the symptoms of many types of autoimmune arthritis.
Eat a balanced diet: A nutritious diet can help you maintain a healthy weight and relieve stress from painful joints.
Aim for a regular sleep schedule: Sleep disturbances can worsen flare-ups and other symptoms.
People with autoimmune arthritis should talk to their doctor about steps they can take to improve their overall health.
Challenge
The long-term effects of autoimmune arthritis can vary depending on the type of disease.
For example, RA can cause joint dysfunction, making it difficult for people to use their arms and legs. People with RA also have a higher risk of heart disease, diabetes, and osteoporosis.
People with arthritis and autoimmune inflammation often find it difficult to maintain a regular work and social schedule.
Sometimes RA patients can develop serious complications that require surgery. There are several surgical options, including joint repair or replacement.
Diagnosing and treating autoimmune arthritis can help reduce complications.
To view the display
Autoimmune arthritis can affect a person’s quality of life. However, there are many treatments that can help people with autoimmune arthritis live healthier and happier lives.
People should talk to their doctor about the best treatment and lifestyle changes for autoimmune arthritis.
















