Health
10 Rashes caused by ulcerative colitis
10 Rashes caused by ulcerative colitis
Ulcerative colitis is a chronic disease that causes inflammation of the large intestine and rectum. It can also cause skin problems.
This article examines how the skin condition relates to ulcerative colitis (UC), a type of inflammatory bowel disease (IBD).
We also discuss how to minimize skin problems during an outbreak and when to see a doctor.
University of California Society of Dermatology
There are several skin conditions associated with ulcerative colitis. They are discussed below.
-
Erythema nodosa
Erythema nodosa is the most common skin condition in people with ulcerative colitis. Erythema nodosa may occur in up to 10% of people with ulcerative colitis.
Erythema nodosum causes painful red nodules that appear on a person’s arms or legs. These nodules look like bruises.
This rash appears during an exacerbation and disappears when the UC is in remission.
-
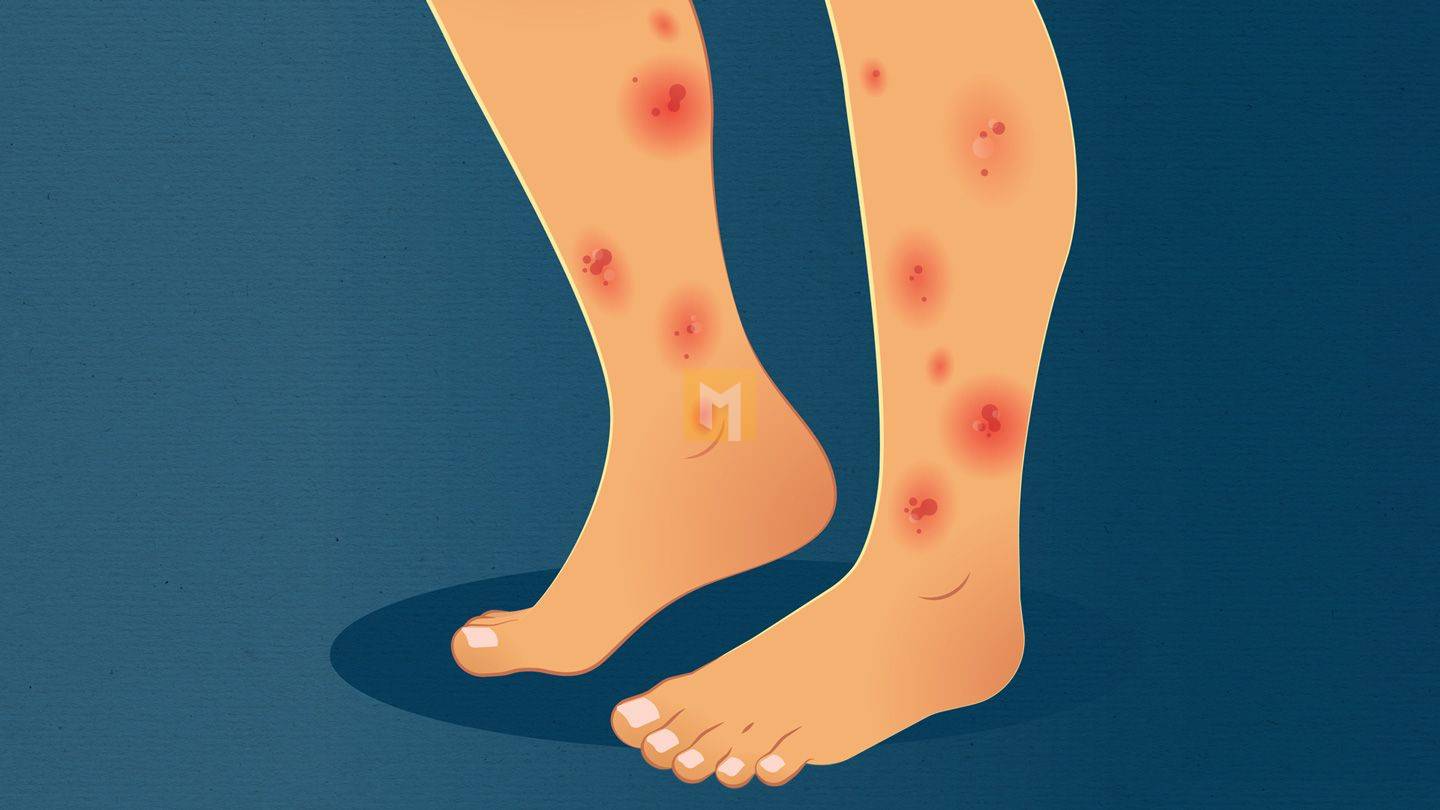
Pyoderma gangrenous
According to a 2012 “Reliable Source” review, pyoderma gangrenosum is the most common skin problem in patients with ulcerative colitis.
The rash begins as a cluster of blisters on the calves, ankles, or hands. It often spreads and can cause deep pain. If you don’t keep it clean, you can get infected.
Researchers believe that the disease is caused by an immune system problem that may be related to ulcerative colitis.
-
Psoriasis
Psoriasis is a skin disease caused by a problem with the immune system. This results in red, blotchy skin with a build-up of dead skin cells.
Ulcerative colitis and other types of inflammatory bowel disease also have psoriasis.
A 2015 study suggested a genetic link between genes that cause IBD and genes that cause psoriasis.
-
Beehives
Hives are raised red spots that can appear anywhere on the body in the form of a rash. They are caused by the reaction of the immune system.
Sometimes it interacts with the medications people take for ulcerative colitis, which can cause chronic hives.
-
Acne
A 2011 authoritative study found a link between taking a drug designed to treat cystic acne (isotretinoin) and ulcerative colitis. More research is needed to better understand this relationship.
-
Irritable bowel syndrome with dermatitis and arthritis.
Bowel-associated cutaneous osteoarthritis syndrome (BADAS) is a condition that causes small bumps on the upper chest and arms, along with other symptoms. These blisters can blister and cause discomfort. BADAS can also damage your feet.
Researchers don’t fully understand, but they think it may be due to inflammation caused by bacteria in the gut. People with inflammatory bowel disease are more likely to be constipated.
-
Vegetative ulcerative dermatitis
Exfoliative dermatitis and exfoliative suppurative dermatitis are two skin disorders.
In the first, red blisters form to form scaly patches on the armpits or groin. Among the latter are pustules in the mouth.
These two conditions are usually combined and called purulent vegetative dermatitis (PPV).
Although this condition is rare, it is associated with UC. Symptoms usually appear after several years of ulcerative colitis. However, ulcerative colitis is often not diagnosed until a doctor diagnoses PPV.
-
Sweet Syndrome
Sweet syndrome is another condition associated with exacerbations of ulcerative colitis.
In people with Sweet’s syndrome, small red or purple spots turn into painful sores on the skin. They mostly appear on the upper extremities, face and neck.
-
Viper
Vitiligo is a skin condition that destroys the cells that produce pigment in the skin. Vitiligo can cause white spots anywhere on the body.
Researchers believe that the cause of vitiligo is an immune disorder. According to the National Institutes of Health (NIH), about 20% of people with vitiligo have another immune disorder, such as UC.
-
Leukocytoclastic vasculitis
Leukocytoclastic vasculitis (hypersensitivity vasculitis) occurs when small blood vessels under the skin become inflamed and die. The inflammatory response causes purple patches of skin on the feet and ankles called purpura.
This condition is caused by inflammation and is associated with flare-ups of loneliness. Leukocytic vasculitis usually resolves when UC goes into remission.
How is cervical inflammation and hives related?
Ulcerative colitis is a painful and uncomfortable inflammatory condition that affects the large intestine and rectum.
When a person has ulcerative colitis, small ulcers appear on the lining of the colon.
The main symptoms of UC are:
- Persistent problems with diarrhea
- Blood, mucus or pus in the stool
- Have frequent bowel movements
- Tiredness
- Anorexia
- Lose weight
Ulcerative colitis attacks
UC is a chronic condition, but can be asymptomatic for weeks or months. This is called remission.
Because people experience many of the symptoms associated with ulcerative colitis, remission periods can be shortened by hypersensitivity.
During a relapse, people with ulcerative colitis may have symptoms similar to those affecting the digestive system.
- rashes or patches of red, swollen skin
- swollen or painful joints
- Stomatitis
- Eyes red and irritated
Why does a rash appear during a skin attack?
Inflammation in the body that causes cervical infections also affects the skin. It causes swelling and a painful rash.
According to a 2015 study, 15% of IBD patients, including those with IBD, have skin problems.
Medicines that a person takes to control the symptoms of ulcerative colitis can also cause skin problems.
It reduces skin problems during skin rashes
Since rheumatoid arthritis patients often have skin problems during flares, the best way to treat skin conditions associated with UC is to administer UC.
Doctors can help people with ulcerative colitis find the best approach for their symptoms and lifestyle.
If blisters develop, the following can help reduce skin problems:
- Taking corticosteroids to reduce inflammation
- eat a balanced diet for healthy skin
- Keep infected skin clean to reduce the risk of infection
- Cover the wound with a bandage
- Take over-the-counter pain relievers
When to see a doctor
If you are particularly concerned about your skin condition, we recommend consulting your doctor for proper diagnosis and treatment.
If skin conditions develop or worsen over time, it’s a good idea to talk to your doctor about how to manage them.
You can also help someone at UCLA find ways to manage their condition holistically.
















