Health
What to know about ulcerative colitis
What to know about ulcerative colitis
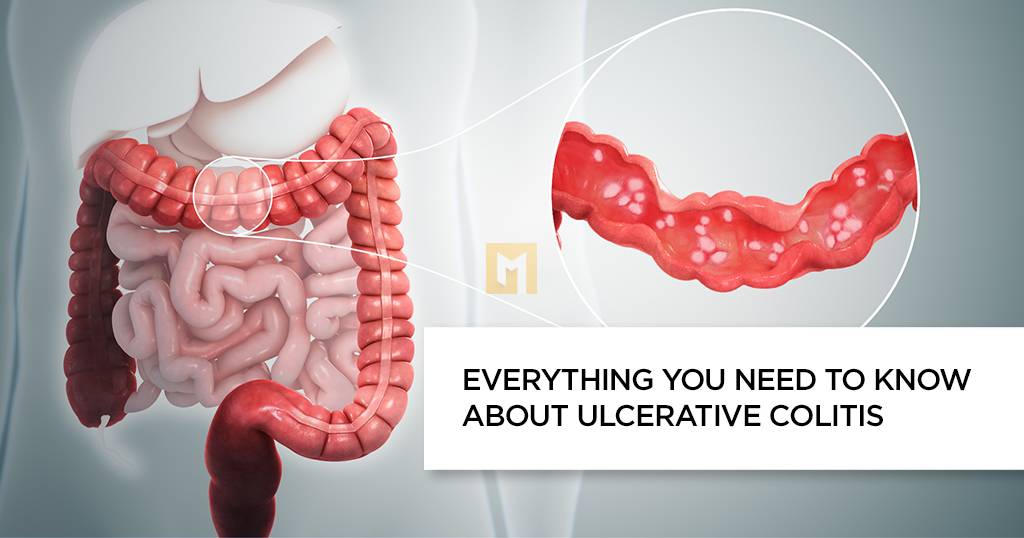
Ulcerative colitis is an infectious disease that causes inflammation of the colon. It is a type of inflammatory bowel disease (IBD) similar to Crohn’s disease.
The large intestine removes nutrients from undigested food and removes waste products in the form of toxins from the rectum and anus.
In severe cases, ulcers appear in the intestinal mucosa. These wounds can bleed, scar and ooze.
There are many drug options, which allows doctors to treat individual needs.
This article discusses ulcerative colitis symptoms, possible causes, and some treatments.
Symptoms
Abdominal pain is often the first symptom of ulcerative colitis.
Some people have excessive liquid stools, abdominal pain and urge to go to the bathroom.
Constipation may start slowly or suddenly. Symptoms depend on the size and degree of the pain.
Common symptoms of ulcerative colitis are:
- Abdominal pain
- bloody diarrhea with mucus
Some may also experience:
- fatigue or exhaustion
- lose weight
- Decreased appetite
- Reduce blood flow
- hot
- dehydration
- Continuous stimulation for elimination
- Symptoms are usually worse in the morning.
However, it often regresses without treatment and depends on the impact of the intestine.
What causes diarrhea?
Symptoms vary depending on the location of the pain.
The following sections describe the different types of ulcerative colitis. Most of them affect different parts of the intestine.
Ulcerative pacitis
This type only affects the end of the large intestine or rectum. Common symptoms include:
- Intestinal bleeding, may be the only symptom
- Back pain
- Most of the time it is impossible to digest food even if it is needed fast
- Ulcerative colitis is usually the mildest type.
Rectosigmoiditis
These include the rectum and the lower end of the large intestine, the sigmoid colon.
Symptoms are:
- Bloody stools
- Abdominal pain
- Abdominal pain
- Continuous stimulation for elimination
- Colitis occurs on the left side
The right side of the rectum and the sigmoid colon and the large intestine are affected.
Common symptoms include:
- Bloody stools
- Abdominal pain on the right side.
- lose weight
- Swadupindadah
It affects the entire stomach. Symptoms are:
- Sometimes stomach pain is very severe
- Abdominal pain and cramping
- tired
- significant weight loss
- Flucortes is a drug
- It is a rare, life-threatening form of colitis that affects the entire colon.
The most common symptoms are severe pain and diarrhea, which can lead to dehydration and shock.
Fulminant colitis can increase the risk of colonic erosion and toxic megacolon.
Food
According to the National Institute of Diabetes, Digestive and Kidney Diseases (NIDDK), several foods can help reduce symptoms, including:
- Eat smaller, more nutritious meals, like 5-6 small meals a day
- Drink plenty of water, especially water, to prevent dehydration
- Avoid caffeine and alcohol, which cause diarrhea
- Avoid carbonated drinks which can cause more fat
- Keep a food diary to determine which foods make your symptoms worse
The doctor may recommend a short-term diet depending on the symptoms, such as:
- A diet low in fiber
- Lactose-free food
- eat a low-fat diet
- Eat less salt
Taking supplements or removing certain foods from your diet may help. But you should consult your doctor before you try supplements or other measures.
Cause
Causes of ulcerative colitis is not known. However, they may include:
Genetic factors
Research shows that people with ulcerative colitis are more likely to have certain genetic traits. A person’s specific genetic makeup can influence the age at which the disease occurs.
Environment
The following environmental factors may contribute to the development of ulcerative colitis:
- Meal
- air pollution
- cigarette smoke
Immunity
The body can respond to a viral or bacterial infection in a way that causes the inflammation associated with ulcerative colitis.
Once the infection is resolved, the immune system continues to respond, causing ongoing inflammation.
Another theory suggests that ulcerative colitis may be an autoimmune disease. A defective immune system can cause inflammation of the colon to fight an infection where it is not present.
Risk
Risk factors for ulcerative colitis include:
Age: Ulcerative colitis can affect people of any age, but it is more common between the ages of 15 and 30.
Ethnicity: Whites and those of Ashkenazi Jewish descent are at greater risk of developing the disease.
Clinical
They will also ask if any close relatives have ever had ulcerative colitis, IBD or Crohn’s disease.
They also check for signs of anemia or low levels of iron in the blood and tenderness around the abdomen.
Several tests can help rule out other possible conditions and diseases, including Crohn’s disease, infections, and irritable bowel syndrome.
This includes:
- blood test
- fecal examination
- X-ray
A barium enema, where a doctor passes a liquid called barium through the colon to show any changes or abnormalities during the scan.
sigmoidoscopy, in which a doctor inserts a flexible tube with a camera on the end called an endoscope into the rectum
Colonoscopy, where the doctor uses an endoscope to examine the entire colon.
CT scan of the abdomen or pelvis
People with ulcerative colitis should see a doctor or gastroenterologist who specializes in treating digestive disorders.
They will assess the type and severity of your condition and devise a treatment plan.
Treatment
Symptoms of ulcerative colitis range from mild to severe, but require treatment. Symptoms may go away without treatment, but they are more likely to return.
Most will receive outpatient treatment. But about 15% of people with the disease have a severe form. Of these, 1 in 5 people may need to spend time in hospital.
The treatment focuses on:
- maintain remission to prevent further symptoms
- The flare is given until the symptoms are relieved.
There are a variety of medications available, and your doctor will create a treatment plan that takes into account your individual needs and wishes. Natural methods can support the treatment, but cannot replace it.
Complications
Potential complications of ulcerative colitis range from nutritional deficiencies to life-threatening rectal bleeding.
Possible complications include:
Colon cancer
Ulcerative colitis increases the risk of colon cancer, especially if symptoms are severe or widespread.
According to NIDDK, the risk of colon cancer is highest when ulcerative colitis affects the entire colon for more than 8 years.
Toxic megacolon
This complication occurs in some cases of severe ulcerative colitis.
In a toxic megacolon, gas is trapped and the rectum swells. When this happens, there is a risk of colon rupture, sepsis and shock.
Vision
The outlook for ulcerative colitis varies widely. Although it is a lifelong disease, experts say that people who have ulcerative colitis have the same mortality rate as those who do not.
















